Patient Develops Allergic Sensitivity to Blood Products Can Recieve Blood Again
| Allergic rhinitis | |
|---|---|
| Other names | Hay fever, pollenosis |
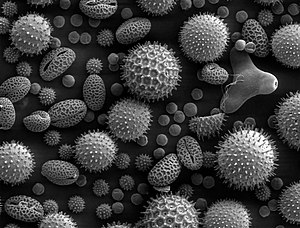 | |
| Pollen grains from a diversity of plants, enlarged 500 times and well-nigh 0.4 mm wide | |
| Specialty | Allergy and immunology |
| Symptoms | Stuffy itchy nose, sneezing, reddish, itchy, and watery eyes, swelling effectually the optics, itchy ears[one] |
| Usual onset | 20 to xl years old[2] |
| Causes | Genetic and environmental factors[3] |
| Adventure factors | Asthma, allergic conjunctivitis, atopic dermatitis[2] |
| Diagnostic method | Based on symptoms, skin prick exam, blood tests for specific antibodies[4] |
| Differential diagnosis | Common cold[3] |
| Prevention | Exposure to animals early on in life[3] |
| Medication | Nasal steroids, antihistamines such as diphenhydramine, cromolyn sodium, leukotriene receptor antagonists such as montelukast, allergen immunotherapy[5] [6] |
| Frequency | ~20% (Western countries)[2] [7] |
Allergic rhinitis, of which the seasonal blazon is called hay fever, is a type of inflammation in the nose that occurs when the immune system overreacts to allergens in the air.[6] Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes.[1] The fluid from the nose is usually clear.[2] Symptom onset is often within minutes post-obit allergen exposure, and can affect slumber and the power to piece of work or report.[2] [viii] Some people may develop symptoms merely during specific times of the twelvemonth, often every bit a issue of pollen exposure.[3] Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.[2]
Allergic rhinitis is typically triggered past environmental allergens such every bit pollen, pet hair, dust, or mold.[3] Inherited genetics and ecology exposures contribute to the development of allergies.[3] Growing up on a farm and having multiple siblings decreases this risk.[2] The underlying mechanism involves IgE antibodies that attach to an allergen, and after result in the release of inflammatory chemicals such as histamine from mast cells.[2] Information technology causes mucous membranes in the olfactory organ, optics and pharynx to get inflamed and itchy every bit they work to eject the allergen. [9]Diagnosis is typically based on a combination of symptoms and a pare prick test or claret tests for allergen-specific IgE antibodies.[four]These tests, however, tin be falsely positive.[4] The symptoms of allergies resemble those of the common cold; nevertheless, they often last for more than two weeks and typically do not include a fever.[3]
Exposure to animals early in life might reduce the gamble of developing these specific allergies.[3] Several different types of medications reduce allergic symptoms, including nasal steroids, antihistamines, such as diphenhydramine, cromolyn sodium, and leukotriene receptor antagonists such equally montelukast.[5] Oftentimes, medications practise non completely control symptoms, and they may also take side effects.[2] Exposing people to larger and larger amounts of allergen, known equally allergen immunotherapy (AIT), is often effective.[6] The allergen tin exist given as an injection under the skin or as a tablet nether the natural language.[6] Treatment typically lasts three to five years, after which benefits may be prolonged.[6]
Allergic rhinitis is the type of allergy that affects the greatest number of people.[10] In Western countries, between 10 and 30% of people are affected in a given year.[2] [vii] It is nearly common between the ages of twenty and xl.[2] The first accurate description is from the tenth-century physician Rhazes.[xi] In 1859, Charles Blackley identified pollen as the cause.[12] In 1906, the machinery was determined by Clemens von Pirquet.[10] The link with hay came about due to an early (and incorrect) theory that the symptoms were brought nigh by the smell of new hay.[13] [14] Although the olfactory property per se is irrelevant, the correlation with hay remains more than random, as elevation hay-harvesting flavor overlaps with summit pollen season, and hay-harvesting work puts people in shut contact with seasonal allergens.
Signs and symptoms [edit]

Illustration depicting inflammation associated with allergic rhinitis
The characteristic symptoms of allergic rhinitis are: rhinorrhea (excess nasal secretion), itching, sneezing fits, and nasal congestion and obstruction.[15] Characteristic physical findings include conjunctival swelling and erythema, eyelid swelling with Dennie–Morgan folds, lower eyelid venous stasis (rings under the optics known as "allergic shiners"), bloated nasal turbinates, and middle ear effusion.[xvi]
There tin likewise be behavioral signs; in order to relieve the irritation or flow of mucus, people may wipe or rub their nose with the palm of their hand in an up motility: an action known as the "nasal salute" or the "allergic salute". This may consequence in a crease running across the nose (or above each nostril if merely one side of the nose is wiped at a fourth dimension), commonly referred to as the "transverse nasal crease", and can pb to permanent physical deformity if repeated enough.[17]
People might too notice that cross-reactivity occurs.[eighteen] For example, people allergic to birch pollen may also find that they have an allergic reaction to the skin of apples or potatoes.[nineteen] A clear sign of this is the occurrence of an itchy throat after eating an apple or sneezing when peeling potatoes or apples. This occurs because of similarities in the proteins of the pollen and the food.[xx] There are many cross-reacting substances. Hay fever is not a truthful fever, meaning information technology does not crusade a cadre trunk temperature in the fever over 37.5–38.3 °C (99.v–100.nine °F).
Cause [edit]
Pollen is oft considered as a cause of allergic rhinitis, hence called Hay fever (See sub-section below).
Predisposing factors to allergic rhinitis include eczema (atopic dermatitis) and asthma. These iii conditions can often occur together which is referred to as the atopic triad.[21] Additionally, ecology exposures such equally air pollution and maternal tobacco smoking tin increase an individual's chances of developing allergies.[21]
[edit]
Allergic rhinitis triggered by the pollens of specific seasonal plants is commonly known equally "hay fever", because it is most prevalent during haying season. Yet, it is possible to accept allergic rhinitis throughout the twelvemonth. The pollen that causes hay fever varies between individuals and from region to region; in full general, the tiny, hardly visible pollens of wind-pollinated plants are the predominant cause. Pollens of insect-pollinated plants are too large to remain airborne and pose no hazard. Examples of plants unremarkably responsible for hay fever include:
- Copse: such as pine (Pinus), mulberry (Morus), birch (Betula), alder (Alnus), cedar (Cedrus), hazel (Corylus), hornbeam (Carpinus), horse anecdote (Aesculus), willow (Salix), poplar (Populus), plane (Platanus), linden/lime (Tilia), and olive (Olea). In northern latitudes, birch is considered to be the most common allergenic tree pollen, with an estimated fifteen–20% of people with hay fever sensitive to birch pollen grains. A major antigen in these is a protein called Bet V I. Olive pollen is most predominant in Mediterranean regions. Hay fever in Japan is caused primarily past sugi (Cryptomeria japonica) and hinoki (Chamaecyparis obtusa) tree pollen.
- "Allergy friendly" copse include: female ash, scarlet maple, xanthous poplar, dogwood, magnolia, double-flowered cherry, fir, spruce, and flowering plum.[22]
- Grasses (Family Poaceae): especially ryegrass (Lolium sp.) and timothy (Phleum pratense). An estimated 90% of people with hay fever are allergic to grass pollen.
- Weeds: ragweed (Ambrosia), plantain (Plantago), nettle/parietaria (Urticaceae), mugwort (Artemisia Vulgaris), Fat hen (Chenopodium), and sorrel/dock (Rumex)
Allergic rhinitis may also be caused past allergy to Balsam of Peru, which is in various fragrances and other products.[23] [24] [25]
Genetic factors [edit]
The causes and pathogenesis of allergic rhinitis are hypothesized to exist affected by both genetic and environmental factors, with many recent studies focusing on specific loci that could be potential therapeutic targets for the affliction. Genome-wide clan studies (GWAS) accept identified a number of different loci and genetic pathways that seem to mediate the trunk'south response to allergens and promote the development of allergic rhinitis, with some of the about promising results coming from studies involving single-nucleotide polymorphisms (SNPs) in the interleukin-33 (IL-33) cistron.[26] [27] The IL-33 poly peptide that is encoded past the IL-33 gene is part of the interleukin family of cytokines that interact with T-helper ii (Th2) cells, a specific type of T cell. Th2 cells contribute to the body'due south inflammatory response to allergens, and specific ST2 receptors, also known as IL1RL1, on these cells bind to the ligand IL-33 protein. This IL-33/ST2 signaling pathway has been found to be one of the main genetic determinants in bronchial asthma pathogenesis, and considering of the pathological linkage between asthma and rhinitis, the experimental focus of IL-33 has now turned to its part in the development of allergic rhinitis in humans and mouse models.[28] Recently, it was establish that allergic rhinitis patients expressed college levels of IL-33 in their nasal epithelium and had a higher concentration of ST2 serum in nasal passageways following their exposure to pollen and other allergens, indicating that this cistron and its associated receptor are expressed at a college rate in allergic rhinitis patients.[29] In a 2020 study on polymorphisms of the IL-33 gene and their link to allergic rhinitis within the Han Chinese population, researchers found that 5 SNPs specifically contributed to the pathogenesis of allergic rhinitis, with three of those five SNPs previously identified every bit genetic determinants for asthma.[30]
Another study focusing on Han Chinese children found that certain SNPs in the protein tyrosine phosphatase non-receptor 22 (PTPN22) gene and cytotoxic T-lymphocyte-associated antigen 4 (CTLA-four) gene tin can be associated with childhood allergic rhinitis and allergic asthma.[31] The encoded PTPN22 poly peptide, which is found primarily in lymphoid tissue, acts as a post-translational regulator by removing phosphate groups from targeted proteins. Importantly, PTPN22 tin can affect the phosphorylation of T jail cell responses, and thus the subsequent proliferation of the T cells. As mentioned earlier, T cells contribute to the body's inflammatory response in a diverseness of ways, and so whatever changes to the cells' construction and part can take potentially deleterious furnishings on the body'southward inflammatory response to allergens. To date, one SNP in the PTPN22 gene has been constitute to be significantly associated with allergic rhinitis onset in children. On the other paw, CTLA-4 is an allowed-checkpoint protein that helps mediate and control the body's immune response to prevent overactivation. It is expressed merely in T cells equally a glycoprotein for the Immunoglobulin (Ig) protein family unit, also known equally antibodies. In that location have been 2 SNPs in CTLA-4 that were found to be significantly associated with childhood allergic rhinitis. Both SNPs nigh likely touch on the associated protein's shape and function, causing the body to showroom an overactive immune response to the posed allergen. The polymorphisms in both genes are only starting time to exist examined, therefore more inquiry is needed to determine the severity of the impact of polymorphisms in the corresponding genes.
Finally, epigenetic alterations and associations are of detail interest to the study and ultimate treatment of allergic rhinitis. Specifically, microRNAs (miRNA) are hypothesized to be imperative to the pathogenesis of allergic rhinitis due to the post-transcriptional regulation and repression of translation in their mRNA complement. Both miRNAs and their common carrier vessel exosomes have been constitute to play a role in the body's immune and inflammatory responses to allergens. miRNAs are housed and packaged within of exosomes until they are ready to be released into the section of the cell that they are coded to reside and act. Repressing the translation of proteins tin ultimately repress parts of the body's immune and inflammatory responses, thus contributing to the pathogenesis of allergic rhinitis and other autoimmune disorders. At that place are many miRNAs that have been deemed potential therapeutic targets for the treatment of allergic rhinitis by many different researchers, with the near widely studied existence miR-133, miR-155, miR-205, miR-498, and let-7e.[27] [32] [33] [34]
Diagnosis [edit]

Allergy testing may reveal the specific allergens to which an individual is sensitive. Skin testing is the about common method of allergy testing.[35] This may include a patch exam to determine if a particular substance is causing the rhinitis, or an intradermal, scratch, or other test. Less commonly, the suspected allergen is dissolved and dropped onto the lower eyelid as a ways of testing for allergies. This exam should exist done only by a physician, since it can be harmful if washed improperly. In some individuals not able to undergo skin testing (as adamant by the medico), the RAST claret test may be helpful in determining specific allergen sensitivity. Peripheral eosinophilia can be seen in differential leukocyte count.
Allergy testing is not definitive. At times, these tests can reveal positive results for certain allergens that are not actually causing symptoms, and can also not selection up allergens that practise crusade an individual'due south symptoms. The intradermal allergy examination is more sensitive than the peel prick exam, just is as well more oft positive in people that exercise not have symptoms to that allergen.[36]
Fifty-fifty if a person has negative pare-prick, intradermal and blood tests for allergies, they may still have allergic rhinitis, from a local allergy in the nose. This is called local allergic rhinitis.[37] Specialized testing is necessary to diagnose local allergic rhinitis.[38]
Classification [edit]
- Seasonal allergic rhinitis (hay fever): Acquired past seasonal peaks in the airborne load of pollens.
- Perennial allergic rhinitis (nonseasonal allergic rhinitis; atopic rhinitis): Caused by allergens nowadays throughout the year (e.g., dander).
Allergic rhinitis may be seasonal, perennial, or episodic.[8] Seasonal allergic rhinitis occurs in particular during pollen seasons. Information technology does not normally develop until later 6 years of age. Perennial allergic rhinitis occurs throughout the year. This type of allergic rhinitis is commonly seen in younger children.[39]
Allergic rhinitis may also be classified as mild-intermittent, moderate-severe intermittent, mild-persistent, and moderate-severe persistent. Intermittent is when the symptoms occur <4 days per week or <4 consecutive weeks. Persistent is when symptoms occur >4 days/week and >4 consecutive weeks. The symptoms are considered balmy with normal sleep, no impairment of daily activities, no damage of piece of work or school, and if symptoms are not troublesome. Severe symptoms result in sleep disturbance, impairment of daily activities, and impairment of schoolhouse or work.[40]
Local allergic rhinitis [edit]
Local allergic rhinitis is an allergic reaction in the nose to an allergen, without systemic allergies. So peel-prick and blood tests for allergy are negative, but in that location are IgE antibodies produced in the nose that react to a specific allergen. Intradermal skin testing may also be negative.[38]
The symptoms of local allergic rhinitis are the same as the symptoms of allergic rhinitis, including symptoms in the eyes. Just as with allergic rhinitis, people can have either seasonal or perennial local allergic rhinitis. The symptoms of local allergic rhinitis tin be mild, moderate, or severe. Local allergic rhinitis is associated with conjunctivitis and asthma.[38]
In 1 written report, almost 25% of people with rhinitis had local allergic rhinitis.[41] In several studies, over 40% of people having been diagnosed with nonallergic rhinitis were constitute to actually take local allergic rhinitis.[37] Steroid nasal sprays and oral antihistamines have been found to exist effective for local allergic rhinitis.[38]
As of 2014, local allergenic rhinitis had mostly been investigated in Europe; in the United states of america, the nasal provocation testing necessary to diagnose the condition was non widely available.[42] : 617
Prevention [edit]
Prevention often focuses on avoiding specific allergens that crusade an private's symptoms. These methods include not having pets, not having carpets or upholstered furniture in the home, and keeping the habitation dry.[43] Specific anti-allergy zippered covers on household items like pillows and mattresses have too proven to be effective in preventing grit mite allergies.[35]
Studies take shown that growing up on a farm and having many older siblings can decrease an individual'southward risk for developing allergic rhinitis.[2]
Studies in immature children take shown that there is higher run a risk of allergic rhinitis in those who have early exposure to foods or formula or heavy exposure to cigarette smoking within the first year of life.[44] [45]
Handling [edit]
The goal of rhinitis handling is to forestall or reduce the symptoms acquired by the inflammation of affected tissues. Measures that are constructive include avoiding the allergen.[15] Intranasal corticosteroids are the preferred medical treatment for persistent symptoms, with other options if this is not effective.[15] Second line therapies include antihistamines, decongestants, cromolyn, leukotriene receptor antagonists, and nasal irrigation.[15] Antihistamines by mouth are suitable for occasional use with mild intermittent symptoms.[15] Mite-proof covers, air filters, and withholding certain foods in babyhood do non have prove supporting their effectiveness.[fifteen]
Antihistamines [edit]
Antihistamine drugs tin be taken orally and nasally to control symptoms such as sneezing, rhinorrhea, itching, and conjunctivitis.
It is best to take oral antihistamine medication before exposure, particularly for seasonal allergic rhinitis. In the case of nasal antihistamines similar azelastine antihistamine nasal spray, relief from symptoms is experienced inside 15 minutes assuasive for a more than immediate 'as-needed' arroyo to dosage. There is not enough testify of antihistamine efficacy every bit an add-on therapy with nasal steroids in the management of intermittent or persistent allergic rhinitis in children, so its adverse effects and boosted costs must be considered.[46]
Ophthalmic antihistamines (such as azelastine in eye drop form and ketotifen) are used for conjunctivitis, while intranasal forms are used mainly for sneezing, rhinorrhea, and nasal pruritus.[47]
Antihistamine drugs tin can have undesirable side-furnishings, the most notable one existence drowsiness in the case of oral antihistamine tablets. Start-generation antihistamine drugs such equally diphenhydramine cause drowsiness, while 2d- and third-generation antihistamines such equally cetirizine and loratadine are less likely to.[47]
Pseudoephedrine is too indicated for vasomotor rhinitis. It is used simply when nasal congestion is present and can be used with antihistamines. In the United states, oral decongestants containing pseudoephedrine must be purchased behind the pharmacy counter in an effort to prevent the manufacturing of methamphetamine.[47] Desloratadine/pseudoephedrine tin as well be used for this condition[ commendation needed ]
Steroids [edit]
Intranasal corticosteroids are used to control symptoms associated with sneezing, rhinorrhea, itching, and nasal congestion.[21] Steroid nasal sprays are constructive and condom, and may exist constructive without oral antihistamines. They take several days to human action and so must be taken continually for several weeks, as their therapeutic event builds up with time.
In 2013, a study compared the efficacy of mometasone furoate nasal spray to betamethasone oral tablets for the handling of people with seasonal allergic rhinitis and constitute that the two have virtually equivalent effects on nasal symptoms in people.[48]
Systemic steroids such as prednisone tablets and intramuscular triamcinolone acetonide or glucocorticoid (such equally betamethasone) injection are effective at reducing nasal inflammation,[ citation needed ] just their utilise is limited by their brusque duration of result and the side-furnishings of prolonged steroid therapy.[49]
Other [edit]
Other measures that may exist used second line include: decongestants, cromolyn, leukotriene receptor antagonists, and nonpharmacologic therapies such equally nasal irrigation.[15]
Topical decongestants may also exist helpful in reducing symptoms such as nasal congestion, simply should not be used for long periods, as stopping them after protracted use can pb to a rebound nasal congestion called rhinitis medicamentosa.
For nocturnal symptoms, intranasal corticosteroids can be combined with nightly oxymetazoline, an adrenergic alpha-agonist, or an antihistamine nasal spray without risk of rhinitis medicamentosa.[50]
Nasal saline irrigation (a do where salt water is poured into the nostrils), may have benefits in both adults and children in relieving the symptoms of allergic rhinitis and it is unlikely to be associated with adverse furnishings.[51]
Allergen immunotherapy [edit]
Allergen immunotherapy (AIT, also termed desensitization) treatment involves administering doses of allergens to accustom the trunk to substances that are generally harmless (pollen, house dust mites), thereby inducing specific long-term tolerance.[52] Allergen immunotherapy is the only treatment that alters the disease mechanism.[53] Immunotherapy can be administered orally (every bit sublingual tablets or sublingual drops), or by injections under the pare (subcutaneous). Subcutaneous immunotherapy is the nearly common form and has the largest body of evidence supporting its effectiveness.[54]
Culling medicine [edit]
There are no forms of complementary or alternative medicine that are evidence-based for allergic rhinitis.[35] Therapeutic efficacy of alternative treatments such as acupuncture and homeopathy is not supported by available evidence.[55] [56] While some show shows that acupuncture is constructive for rhinitis, specifically targeting the sphenopalatine ganglion acupoint, these trials are however limited.[57] Overall, the quality of testify for complementary-alternative medicine is not strong enough to be recommended by the American Academy of Allergy, Asthma and Immunology.[35] [58]
Epidemiology [edit]
Allergic rhinitis is the type of allergy that affects the greatest number of people.[10] In Western countries, between 10 and thirty percent of people are affected in a given year.[ii] It is most common between the ages of twenty and 40.[two]
History [edit]
The start accurate description is from the 10th century medico Rhazes.[11] Pollen was identified as the cause in 1859 past Charles Blackley.[12] In 1906 the mechanism was determined by Clemens von Pirquet.[10] The link with hay came about due to an early (and wrong) theory that the symptoms were brought most by the smell of new hay.[xiii] [14]
References [edit]
- ^ a b "Ecology Allergies: Symptoms". NIAID. April 22, 2015. Archived from the original on June 18, 2015. Retrieved June 19, 2015.
- ^ a b c d eastward f chiliad h i j k l m n Wheatley LM, Togias A (January 2015). "Clinical practice. Allergic rhinitis". The New England Journal of Medicine. 372 (5): 456–63. doi:x.1056/NEJMcp1412282. PMC4324099. PMID 25629743.
- ^ a b c d e f thousand h "Crusade of Environmental Allergies". NIAID. Apr 22, 2015. Archived from the original on June 17, 2015. Retrieved June 17, 2015.
- ^ a b c "Environmental Allergies: Diagnosis". NIAID. May 12, 2015. Archived from the original on June 17, 2015. Retrieved June 19, 2015.
- ^ a b "Environmental Allergies: Treatments". NIAID. April 22, 2015. Archived from the original on June 17, 2015. Retrieved June 17, 2015.
- ^ a b c d e "Immunotherapy for Environmental Allergies". NIAID. May 12, 2015. Archived from the original on June 17, 2015. Retrieved June 19, 2015.
- ^ a b Dykewicz MS, Hamilos DL (February 2010). "Rhinitis and sinusitis". The Journal of Allergy and Clinical Immunology. 125 (2 Suppl 2): S103-15. doi:10.1016/j.jaci.2009.12.989. PMID 20176255.
- ^ a b Covar R (2018). "Allergic Disorders". Current Diagnosis & Treatment: Pediatrics (24th ed.). NY: McGraw-Hill. ISBN978-1-259-86290-8.
- ^ "Allergic Rhinitis (Hay Fever): Symptoms, Diagnosis & Treatment". Cleveland Dispensary . Retrieved March 23, 2022.
- ^ a b c d Fire fighter P (2002). Pediatric otolaryngology vol 2 (fourth ed.). Philadelphia, Pa.: W. B. Saunders. p. 1065. ISBN9789997619846.
- ^ a b Colgan R (2009). Advice to the young doctor on the art of medicine. New York: Springer. p. 31. ISBN9781441910349. Archived from the original on September 8, 2017.
- ^ a b Justin Parkinson (July i, 2014). "John Bostock: The man who 'discovered' hay fever". BBC News Magazine. Archived from the original on July 31, 2015. Retrieved June 19, 2015.
- ^ a b Hall M (May xix, 1838). "Dr. Marshall Hall on Diseases of the Respiratory System; III. Hay Asthma". The Lancet. 30 (768): 245. doi:10.1016/S0140-6736(02)95895-2.
With respect to what is termed the heady cause of the disease, since the attention of the public has been turned to the subject an idea has very more often than not prevailed, that information technology is produced past the fetor from new hay, and it has hence obtained the pop name of hay fever. [...] the effluvium from hay has no connection with the disease.
- ^ a b History of Allergy. Karger Medical and Scientific Publishers. 2014. p. 62. ISBN9783318021950. Archived from the original on June ten, 2016.
- ^ a b c d e f g Sur DK, Plesa ML (December 2015). "Treatment of Allergic Rhinitis". American Family unit Physician. 92 (11): 985–92. PMID 26760413. Retrieved April 21, 2018.
- ^ Valet RS, Fahrenholz JM (2009). "Allergic rhinitis: update on diagnosis". Consultant. 49: 610–3. Archived from the original on January 14, 2010.
- ^ Pray WS (2005). Nonprescription Product Therapeutics. Lippincott Williams & Wilkins. p. 221. ISBN978-0781734981.
- ^ Czaja-Bulsa M, Bachórska J (December 1998). "[Food allergy in children with pollinosis in the Western sea declension region]" [Nutrient allergy in children with pollinosis in the Western sea declension region]. Polski Merkuriusz Lekarski (in Polish). 5 (30): 338–40. PMID 10101519.
- ^ Yamamoto T, Asakura K, Shirasaki H, Himi T, Ogasawara H, Narita S, Kataura A (October 2005). "[Relationship betwixt pollen allergy and oral allergy syndrome]" [Relationship between Pollen Allergy and Oral Allergy Syndrome]. Nihon Jibiinkoka Gakkai Kaiho (in Japanese). 108 (10): 971–ix. doi:10.3950/jibiinkoka.108.971. PMID 16285612.
- ^ Malandain H (September 2003). "[Allergies associated with both food and pollen]" [Allergies associated with both food and pollen]. European Annals of Allergy and Clinical Immunology (in French). 35 (7): 253–6. PMID 14626714. INIST:15195402.
- ^ a b c Cahill One thousand (2018). "Urticaria, Angioedema, and Allergic Rhinitis." 'Harrison's Principles of Internal Medicine (20th ed.). NY: McGraw-Hill. pp. Affiliate 345. ISBN978-1-259-64403-0.
- ^ "Allergy Friendly Trees". Forestry.most.com. March 5, 2014. Archived from the original on April fourteen, 2014. Retrieved April 25, 2014.
- ^ Pamela Brooks (2012). The Daily Telegraph: Consummate Guide to Allergies. ISBN9781472103949 . Retrieved Apr 27, 2014.
- ^ Denver Medical Times: Utah Medical Journal. Nevada Medicine. January 1, 2010. Archived from the original on September 8, 2017. Retrieved April 27, 2014.
- ^ George Clinton Andrews; Anthony Nicholas Domonkos (July i, 1998). Diseases of the Skin: For Practitioners and Students. Archived from the original on September 8, 2017. Retrieved April 27, 2014.
- ^ Kamekura R, Kojima T, Takano Thousand, Go M, Sawada North, Himi T (2012). "The Role of IL-33 and Its Receptor ST2 in Human being Nasal Epithelium with Allergic Rhinitis". Clin Exp Allergy. 42 (two): 218–228. doi:10.1111/j.1365-2222.2011.03867.ten. PMID 22233535. S2CID 21799632.
- ^ a b Zhang XH, Zhang YN, Liu Z (2014). "MicroRNA in Chronic Rhinosinusitis and Allergic Rhinitis". Curr Allergy Asthma Rep. 14 (2): 415. doi:10.1007/s11882-013-0415-three. PMID 24408538. S2CID 39239208.
- ^ Baumann R, Rabaszowski Yard, Stenin I, Tilgner Fifty, Gaertner-Akerboom M, Scheckenbach K, Wiltfang J, Chaker A, Schipper J, Wagenmann K (2013). "Nasal Levels of Soluble IL-33R ST2 and IL-16 in Allergic Rhinitis: Inverse Correlation Trends with Disease Severity". Clin Exp Allergy. 43 (10): 1134–1143. doi:10.1111/cea.12148. PMID 24074331. S2CID 32689683.
- ^ Ran H, Xiao H, Zhou Ten, Guo L, Lu S (2020). "Unmarried-Nucleotide Polymorphisms and Haplotypes in the Interleukin-33 Gene Are Associated with a Risk of Allergic Rhinitis in the Chinese Population". Exp Ther Med. 20 (five): 102. doi:ten.3892/etm.2020.9232. PMC7506885. PMID 32973951.
- ^ Ran, He; Xiao, Hua; Zhou, Xing; Guo, Lijun; Lu, Shuang (November 2020). "Single-nucleotide polymorphisms and haplotypes in the interleukin-33 gene are associated with a risk of allergic rhinitis in the Chinese population". Experimental and Therapeutic Medicine. 20 (5): 102. doi:10.3892/etm.2020.9232. ISSN 1792-0981. PMC7506885. PMID 32973951.
- ^ Song SH, Wang XQ, Shen Y, Hong SL, Ke, X. "Association betwixt PTPN22/CTLA-4 Factor Polymorphism and Allergic Rhinitis with Asthma in Children". Iranian Journal of Allergy, Asthma and Immunology: 413–419.
- ^ Suojalehto H, Toskala E, Kilpeläinen M, Majuri ML, Mitts C, Lindström I, Puustinen A, Plosila T, Sipilä J, Wolff H, Alenius H (2013). "MicroRNA Profiles in Nasal Mucosa of Patients with Allergic and Nonallergic Rhinitis and Asthma". International Forum of Allergy and Rhinology. 3 (8): 612–620. doi:x.1002/alr.21179. PMID 23704072. S2CID 29759402.
- ^ Sastre B, Cañas JA, Rodrigo-Muñoz JM, del Pozo V (2017). "Novel Modulators of Asthma and Allergy: Exosomes and MicroRNAs". Forepart Immunol. 8: 826. doi:10.3389/fimmu.2017.00826. PMC5519536. PMID 28785260.
- ^ Xiao L, Jiang L, Hu Q, Li Y. "MicroRNA-133b Ameliorates Allergic Inflammation and Symptom in Murine Model of Allergic Rhinitis by Targeting NIrp3". CPB. 42 (3): 901–912.
- ^ a b c d "American Academy of Allergy Asthma and Immunology".
- ^ "Allergy Tests". Archived from the original on Jan 14, 2012.
- ^ a b Rondón C, Canto Thousand, Blanca M (February 2010). "Local allergic rhinitis: a new entity, characterization and further studies". Current Opinion in Allergy and Clinical Immunology. 10 (ane): one–7. doi:x.1097/ACI.0b013e328334f5fb. PMID 20010094. S2CID 3472235.
- ^ a b c d Rondón C, Fernandez J, Canto Chiliad, Blanca Yard (2010). "Local allergic rhinitis: concept, clinical manifestations, and diagnostic approach". Journal of Investigational Allergology & Clinical Immunology. 20 (5): 364–71, quiz ii p post-obit 371. PMID 20945601.
- ^ "Rush Academy Medical Center". Archived from the original on February xix, 2015. Retrieved March 5, 2008.
- ^ Bousquet J, Reid J, van Weel C, Baena Cagnani C, Canonica GW, Demoly P, et al. (Baronial 2008). "Allergic rhinitis management pocket reference 2008". Allergy. 63 (eight): 990–6. doi:10.1111/j.1398-9995.2008.01642.x. PMID 18691301. S2CID 11933433.
- ^ Rondón C, Campo P, Galindo Fifty, Blanca-López Due north, Cassinello MS, Rodriguez-Bada JL, et al. (Oct 2012). "Prevalence and clinical relevance of local allergic rhinitis". Allergy. 67 (10): 1282–8. doi:10.1111/all.12002. PMID 22913574. S2CID 22470654.
- ^ Flintstone Pow, Haughey BH, Robbins KT, Thomas JR, Niparko JK, Lund VJ, Lesperance MM (Nov 28, 2014). Cummings Otolaryngology – Head and Neck Surgery Eastward-Book. Elsevier Health Sciences. ISBN9780323278201.
- ^ "Prevention". nhs.uk. Oct iii, 2018. Retrieved Feb 17, 2019.
- ^ Akhouri S, House SA. Allergic Rhinitis. [Updated 2020 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://world wide web.ncbi.nlm.nih.gov/books/NBK538186/
- ^ Skoner DP (July 2001). "Allergic rhinitis: definition, epidemiology, pathophysiology, detection, and diagnosis". The Journal of Allergy and Clinical Immunology. 108 (i Suppl): S2-8. doi:10.1067/mai.2001.115569. PMID 11449200.
- ^ Nasser M, Fedorowicz Z, Aljufairi H, McKerrow West (July 2010). "Antihistamines used in addition to topical nasal steroids for intermittent and persistent allergic rhinitis in children". The Cochrane Database of Systematic Reviews (vii): CD006989. doi:10.1002/14651858.CD006989.pub2. PMC7388927. PMID 20614452.
- ^ a b c May JR, Smith PH (2008). "Allergic Rhinitis". In DiPiro JT, Talbert RL, Yee GC, Matzke Thou, Wells B, Posey LM (eds.). Pharmacotherapy: A Pathophysiologic Approach (7th ed.). New York: McGraw-Hill. pp. 1565–75. ISBN978-0071478991.
- ^ Karaki M, Akiyama K, Mori Due north (June 2013). "Efficacy of intranasal steroid spray (mometasone furoate) on treatment of patients with seasonal allergic rhinitis: comparison with oral corticosteroids". Auris, Nasus, Larynx. 40 (three): 277–81. doi:10.1016/j.anl.2012.09.004. PMID 23127728.
- ^ Ohlander BO, Hansson RE, Karlsson KE (1980). "A comparison of 3 injectable corticosteroids for the treatment of patients with seasonal hay fever". The Periodical of International Medical Research. eight (1): 63–9. doi:10.1177/030006058000800111. PMID 7358206. S2CID 24169670.
- ^ Baroody FM, Brown D, Gavanescu L, DeTineo Grand, Naclerio RM (April 2011). "Oxymetazoline adds to the effectiveness of fluticasone furoate in the handling of perennial allergic rhinitis". The Periodical of Allergy and Clinical Immunology. 127 (4): 927–34. doi:ten.1016/j.jaci.2011.01.037. PMID 21377716.
- ^ Caput K, Snidvongs One thousand, Glew S, Scadding Yard, Schilder AG, Philpott C, Hopkins C (June 2018). "Saline irrigation for allergic rhinitis". The Cochrane Database of Systematic Reviews. 2018 (6): CD012597. doi:10.1002/14651858.CD012597.pub2. PMC6513421. PMID 29932206.
- ^ Van Overtvelt L, Batard T, Fadel R, Moingeon P (Dec 2006). "Mécanismes immunologiques de fifty'immunothérapie sublinguale spécifique des allergènes". Revue Française d'Allergologie et d'Immunologie Clinique. 46 (viii): 713–720. doi:10.1016/j.allerg.2006.10.006.
- ^ Creticos P. "Subcutaneous immunotherapy for allergic disease: Indications and efficacy". UpToDate.
- ^ Calderon MA, Alves B, Jacobson M, Hurwitz B, Sheikh A, Durham S (Jan 2007). "Allergen injection immunotherapy for seasonal allergic rhinitis". The Cochrane Database of Systematic Reviews (i): CD001936. doi:10.1002/14651858.CD001936.pub2. PMC7017974. PMID 17253469.
- ^ Passalacqua G, Bousquet PJ, Carlsen KH, Kemp J, Lockey RF, Niggemann B, et al. (May 2006). "ARIA update: I—Systematic review of complementary and alternative medicine for rhinitis and asthma". The Journal of Allergy and Clinical Immunology. 117 (v): 1054–62. doi:10.1016/j.jaci.2005.12.1308. PMID 16675332.
- ^ Terr AI (2004). "Unproven and controversial forms of immunotherapy". Clinical Allergy and Immunology. 18: 703–10. PMID 15042943.
- ^ Fu Q, Zhang Fifty, Liu Y, Li X, Yang Y, Dai One thousand, Zhang Q (March 12, 2019). "Effectiveness of Acupuncturing at the Sphenopalatine Ganglion Acupoint Alone for Treatment of Allergic Rhinitis: A Systematic Review and Meta-Analysis". Evidence-Based Complementary and Alternative Medicine. 2019: 6478102. doi:10.1155/2019/6478102. PMC6434301. PMID 30992709.
- ^ Witt CM, Brinkhaus B (Oct 2010). "Efficacy, effectiveness and cost-effectiveness of acupuncture for allergic rhinitis – An overview virtually previous and ongoing studies". Autonomic Neuroscience. 157 (1–2): 42–5. doi:ten.1016/j.autneu.2010.06.006. PMID 20609633. S2CID 31349218.
External links [edit]
- Allergic rhinitis at Curlie
Source: https://en.wikipedia.org/wiki/Allergic_rhinitis
0 Response to "Patient Develops Allergic Sensitivity to Blood Products Can Recieve Blood Again"
Post a Comment